New immunotherapy shows promise for treating neuroblastoma
A novel CAR T-cell therapy designed to target cancerous tumours has shown promising early results in treating children with neuroblastoma.
Neuroblastoma is one of the most common cancers in childhood and it can be difficult to treat. Around half of the children diagnosed have aggressive, high-risk neuroblastoma and need very intensive treatment, including high-dose chemotherapy, surgery and radiotherapy. Despite all of this, the cancer comes back in around 40-50% of children with high-risk neuroblastoma and only 50% survive long-term.
A novel CAR T-cell therapy designed to target cancerous tumours has shown promising early results in treating children with neuroblastoma. The original pre-clinical work was funded by Neuroblastoma UK to help launch the study. It was taken forward to clinical trial sponsored by Cancer Research UK and supported by UCL Great Ormond Street Biomedical Research Centre, starting in 2016 and completed in 2020.
Dr Karin Straathof is one of the lead investigators on the study and clinician at Great Ormond Street Hospital.
Dr Karin Straathof tells us more.
“Quite simply, this research wouldn’t have happened without the support and funds from Neuroblastoma UK when we first started our investigations..”
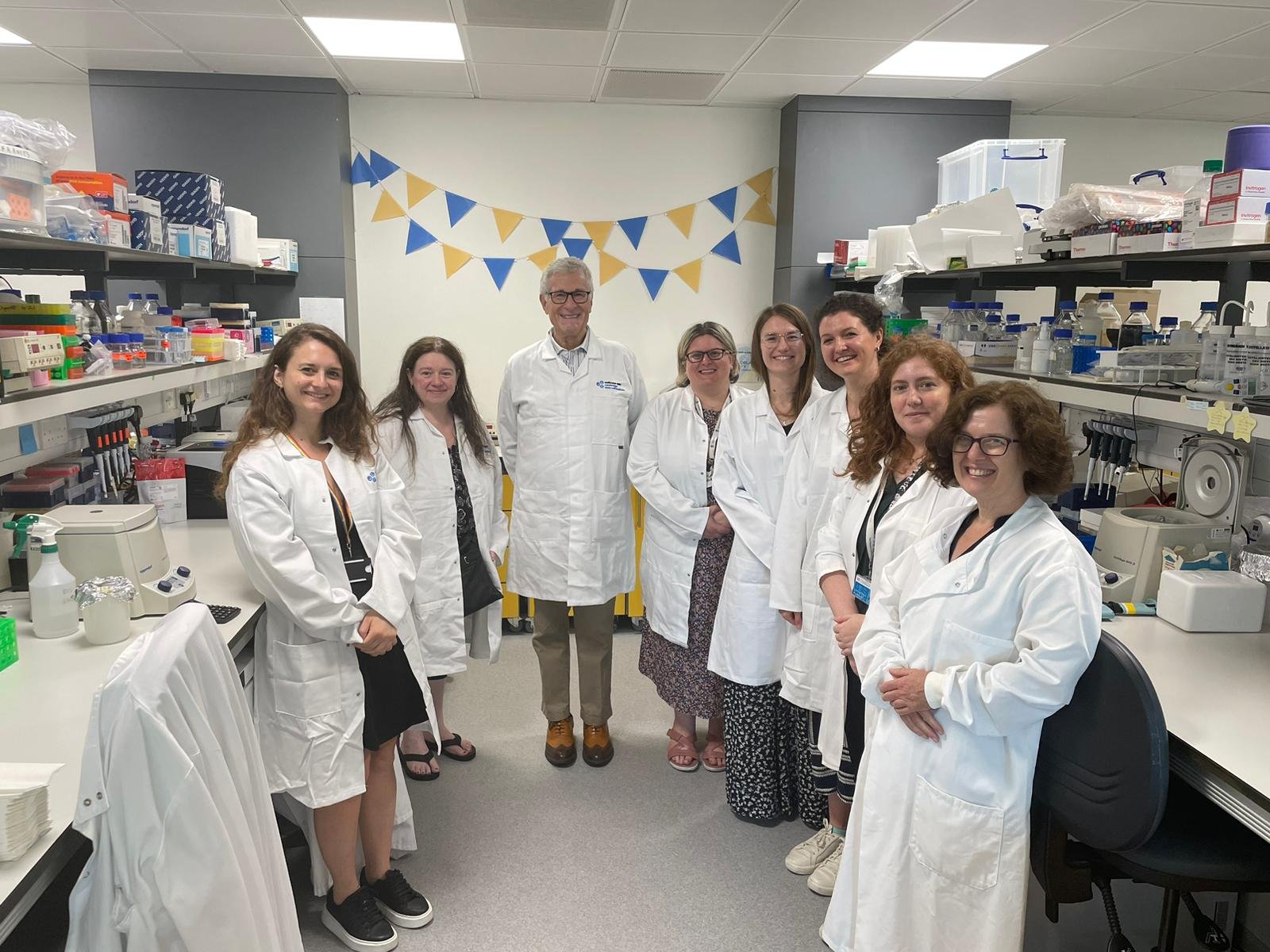
Dr Karin Straathof in the research lab.
Simply giving children more of the same treatment may not give us better results. We need new treatments to work in a different way for it to work better. It’s taken 15 years or so of research and trials, but by developing a CAR T-cell therapy specifically for neuroblastoma, we can provide a much-needed new treatment for children.
With CAR T-cell therapy we take advantage of our immune system. Our immune system is fascinating. It’s job is to keep us safe from infection and it can tell the difference between abnormal, infected cells and healthy cells. By understanding more about how our immune system works, we can develop kinder, more effective treatment for children with neuroblastoma.
What is CAR T-cell therapy and how can it help children with neuroblastoma?
“We wanted to know whether we could reprogramme the T-cells with new ‘instructions’, so that they can distinguish between healthy cells and cancer cells, and leave the healthy cells alone.”
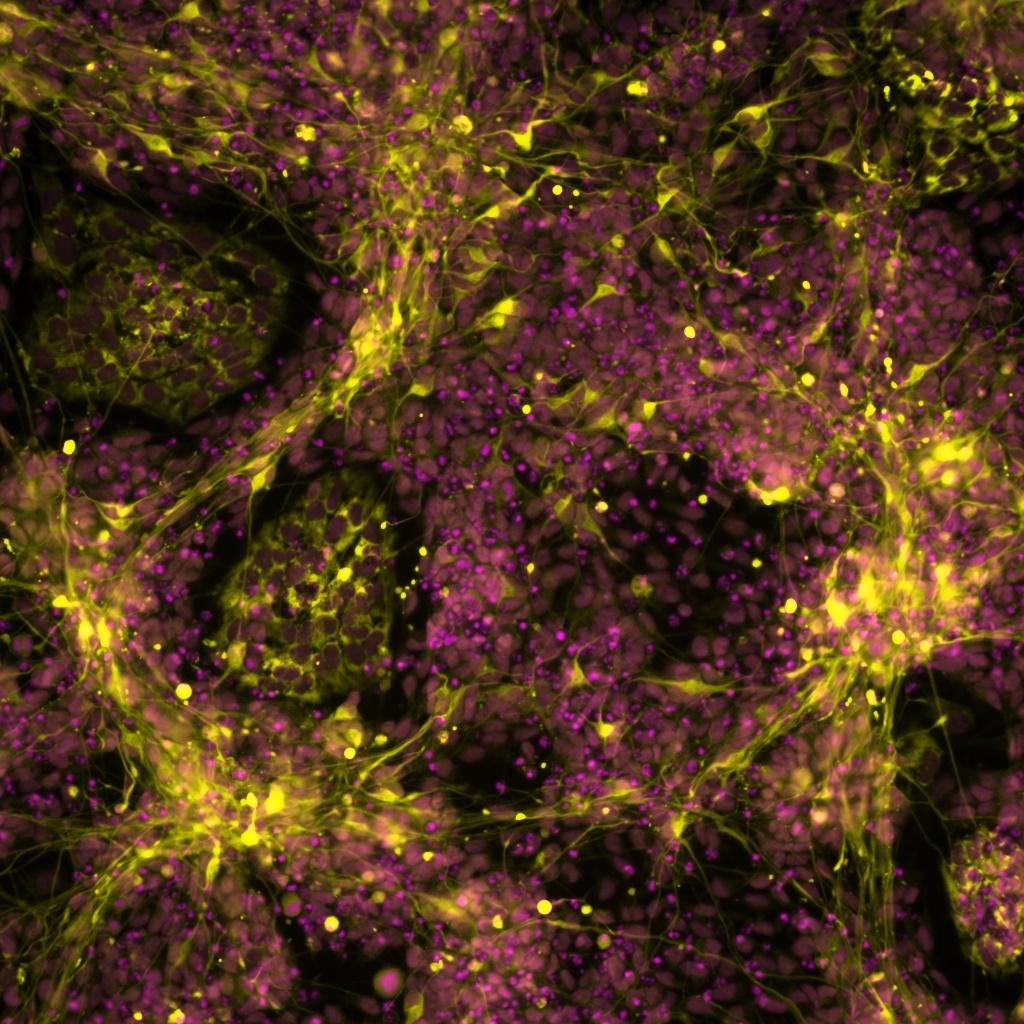
An image of a CAR T-cell
A T-cell is a type of immune cell. A treatment called CAR T-cell immunotherapy takes a patient's T-cells and modifies them to contain a molecule called a chimeric antigen receptor (CAR).
These CAR T-cells can then recognise and kill cancer cells. CAR T-cell therapy was first used to treat blood cancers. It worked so well that it is now part of the standard protocol for patients with difficult to treat blood cancers. So we were curious - could this same process be used to treat children with neuroblastoma?
The difficulty we have is that cancer cells have evolved from previously healthy cells, so it is harder for T-cells to tell them apart from healthy cells. This is particularly true for solid tumours like neuroblastomas. We wanted to know whether we could reprogramme the T-cells with new ‘instructions’, so that they can distinguish between healthy cells and cancer cells, and leave the healthy cells alone.
To be able to do this we had to use something that is present on neuroblastoma cells but not on healthy parts of our bodies for the T-cell to recognise. And that something was the GD2 molecule on the surface on a neuroblastoma cell (we already use GD2 in antibody treatment as a marker to recognise the neuroblastoma). We then harvested blood cells from neuroblastoma patients and genetically modified them in the lab with the CAR receptor to equip them with new instructions how to recognise the GD2 molecule.
What happened in the Phase One clinical trial?
“This clinical trial was one of the first trials where CAR T-cells were used to treat a cancer that wasn’t a blood cancer. ”
This clinical trial was one of the first trials where CAR T-cells were used to treat a cancer that wasn’t a blood cancer. We needed to know how many of the modified cells to give a child with neuroblastoma and whether they needed pre-treatment chemotherapy. This brief chemotherapy would deplete a child’s own immune cells so that we could give the new, modified cells space to settle, divide and work more effectively.
12 children with relapsed or refractory neuroblastoma were treated as part of the clinical trial, with six patients receiving higher amounts of CAR T-cells. In three of these patients, there was some evidence that the modified cells were having an impact. We found that the cells would start to divide and stay around in the blood. The T-cells would then be activated, the immune system would start to work and neuroblastoma tumour cells were cleared up. But it was a short effect. The CAR T-cells seemed to run out of steam and depleted, eventually disappearing and the neuroblastoma would come back.
What happens next?
“...the CARs give the T-cells power and now adding more engineering modules will give them ‘super power’ - an extra kick to work better!”
We’ve come full circle. A great deal was learnt from the study about what worked well, and the outcomes gave us new ideas to investigate. In 2019, we received a further research grant of £154,491 from Neuroblastoma UK to develop the study further.
We now know that neuroblastoma puts up barriers to stop the immune system from working, so we have started to unpick what those barriers are. We are now using next generation CAR T-cells with additional reprogramming; we already know how to engineer the cells to recognise GD2 molecules, and we now also introduce more instructions to make the T-cells work better, despite these barriers. You can say the CARs give the T-cells power and now adding more engineering modules will give them ‘super power’ - an extra kick to work better!
Understanding which is the best method and which modules to incorporate is what we are currently working on. We will then use these ‘super’ CAR T-cells in a new clinical trial, but there is a lot of work to do before we get to that stage!
How did Neuroblastoma UK support this project?
Quite simply, this research wouldn’t have happened without the support and funds from Neuroblastoma UK when we first started our investigations.
Neuroblastoma UK made a huge contribution to this project, donating £200,000 in 2013 at the very beginning. It was really important to have funding at this early stage when we needed to take forward research from what we knew about leukaemia to treat neuroblastoma. It then helped us to leverage additional funding further down the line.
And of course the further funding in 2019 from Neuroblastoma UK will help us to develop the study further.
Why did you choose to research neuroblastoma?
I want children to be cured of neuroblastoma and to live a happy, healthy life. As a paediatric oncologist at Great Ormond Street Hospital, my research has been inspired by seeing children and their families on the ward. These young patients have really intensive treatment and spend lots of time in hospital, so we really need to come up with different, kinder ways to treat them and reduce the long-term side effects.
What motivates you in your role?
I am fascinated by how clever and fine tuned our immune system is. It’s a dynamic system and I am intrigued by how we can take advantage of this to treat cancer. As soon as I started training in paediatrics and paediatric oncology, I wanted to start working on immunotherapy as a cancer treatment.
FUNDING RESEARCH. SAVING LIVES.
At Neuroblastoma UK, we fund leading research to help scientists like Dr Straathof to develop new, effective and kinder treatments for children with neuroblastoma.
But we can only do this with your support. Your gift could help increase children’s chance of survival, but also help them to thrive in the future.
And with more money for cutting-edge research, we could find a cure for neuroblastoma sooner. Please donate today and help fight childhood cancer.








Neuroblastoma UK is awarding £1.1 million in its 2024 grant round to fund new innovative research into neuroblastoma. New therapeutic approaches, pathways to improve existing treatments and exploration of an MRNA vaccine are just some of the projects to be funded in the 2024 grant round; with an emphasis on translational research which can be rapidly transferred from the lab bench to bedside.