Current research projects
As part of Neuroblastoma UK’s 2024 Grant Round, Professor Steve Archibald and his team at King’s College London received £268,301 to conduct research into improving the availability of scanning drugs to optimise radiation dose administered in children with neuroblastoma.
In 2021, Neuroblastoma UK awarded £469,093 in research funding to an international team of leading clinician-scientists to explore how blood tests (biomarker testing) could be used in clinical trials to improve outcomes for children with neuroblastoma.
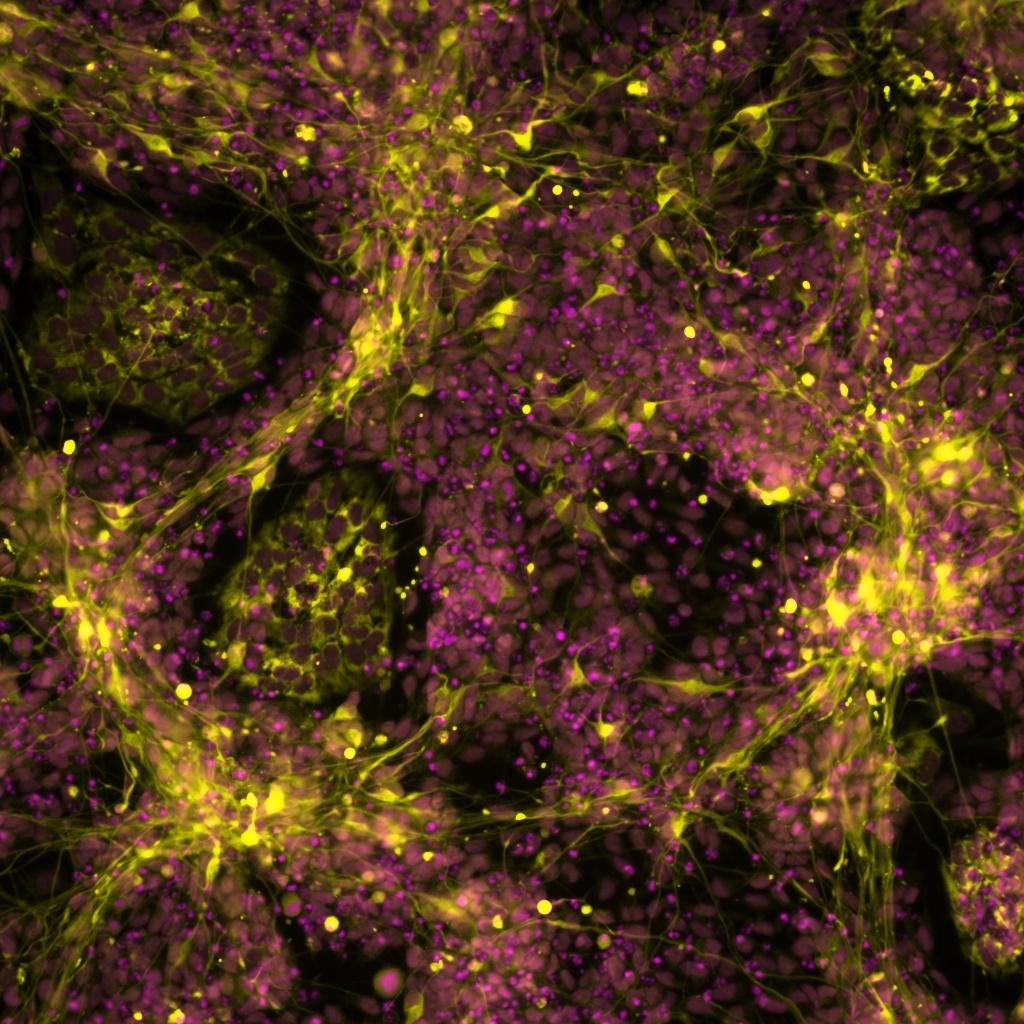
Researchers from the University of Sheffield and St. Anna Children’s Cancer Research Institute have created a model designed to investigate the origins of neuroblastoma, a cancer primarily affecting infants and young children. The findings offer hope for the creation of tailored treatments which treat aggressive neuroblastomas and minimise the adverse effects experienced by patients from existing therapies.
In 2023, Dr Gao, working with Prof Juliet Gray and Dr Zoë Walters at the University of Southampton, aimed to determine the role of natural killer cell- mediated anti-tumour effects in neuroblastoma, after treatment with EZH2. The objectives of the study were to look at the correlation between EZH2 protein expression and the surface expression of natural killer ligands in neuroblastoma cells, and to determine if the natural killer cells induced cytotoxicity that could be enhanced in the neuroblastoma cell lines with EZH2 inhibitors.
This year we reviewed the current results of the research initially funded by Neuroblastoma UK from 2010 to 2017. Our Symposiums over the last ten years have brought together researchers to share their work and highlight topics, examples are: new treatments, advances in differentiation therapy, genetic landscape of neuroblastoma , the role of MYC gene and micro RNA signatures.





Neuroblastoma UK is awarding £1.1 million in its 2024 grant round to fund new innovative research into neuroblastoma. New therapeutic approaches, pathways to improve existing treatments and exploration of an MRNA vaccine are just some of the projects to be funded in the 2024 grant round; with an emphasis on translational research which can be rapidly transferred from the lab bench to bedside.